Overview
Adult acquired flatfoot deformity (AAFD) is a painful, chronic condition found most often in women between the ages of 40 and 60. AAFD occurs when the soft tissues of the foot are overstretched and torn, causing the arch to collapse. Flatfoot deformities may also be caused by a foot fracture, or may result from long-term arthritis. Once the posterior tibial tendon-the tendon unit that holds up the arch-loses its function, the foot becomes ?flat? as the bones spread out of position during weight bearing. Without an AAFD repair, the condition may progress until the affected foot becomes entirely rigid and quite painful.
Causes
There are numerous causes of acquired adult flatfoot, including fracture or dislocation, tendon laceration, tarsal coalition, arthritis, neuroarthropathy, neurologic weakness, and iatrogenic causes. The most common cause of acquired adult flatfoot is posterior tibial tendon dysfunction.
Symptoms
Depending on the cause of the flatfoot, a patient may experience one or more of the different symptoms here. Pain along the course of the posterior tibial tendon which lies on the inside of the foot and ankle. This can be associated with swelling on the inside of the ankle. Pain that is worse with activity. High intensity or impact activities, such as running, can be very difficult. Some patients can have difficulty walking or even standing for long periods of time. When the foot collapses, the heel bone may shift position and put pressure on the outside ankle bone (fibula). This can cause pain on the outside of the ankle. Arthritis in the heel also causes this same type of pain. Patients with an old injury or arthritis in the middle of the foot can have painful, bony bumps on the top and inside of the foot. These make shoewear very difficult. Occasionally, the bony spurs are so large that they pinch the nerves which can result in numbness and tingling on the top of the foot and into the toes. Diabetics may only notice swelling or a large bump on the bottom of the foot. Because their sensation is affected, people with diabetes may not have any pain. The large bump can cause skin problems and an ulcer (a sore that does not heal) may develop if proper diabetic shoewear is not used.
Diagnosis
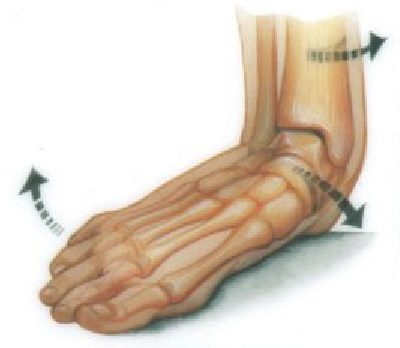
Perform a structural assessment of the foot and ankle. Check the ankle for alignment and position. When it comes to patients with severe PTTD, the deltoid has failed, causing an instability of the ankle and possible valgus of the ankle. This is a rare and difficult problem to address. However, if one misses it, it can lead to dire consequences and potential surgical failure. Check the heel alignment and position of the heel both loaded and during varus/valgus stress. Compare range of motion of the heel to the normal contralateral limb. Check alignment of the midtarsal joint for collapse and lateral deviation. Noting the level of lateral deviation in comparison to the contralateral limb is critical for surgical planning. Check midfoot alignment of the naviculocuneiform joints and metatarsocuneiform joints both for sag and hypermobility.
Non surgical Treatment
The adult acquired flatfoot is best treated early. Accurate assessment by your doctor will determine which treatment is suitable for you. Reduce your level of activity and follow the RICE regime. R - rest as often as you are able. Refrain from activity that will worsen your condition, such as sports and walking. I - ice, apply to the affected area, ensure you protect the area from frostbite by applying a towel over the foot before using the ice pack. C - compression, a Tubigrip or elasticated support bandage may be applied to relieve symptoms and ease pain and discomfort. E - elevate the affected foot to reduce painful swelling. You will be prescribed pain relief in the form of non-steroidal antiinflammatory medications (if you do not suffer with allergies or are asthmatic). Immobilisation of your affected foot - this will involve you having a below the knee cast for four to eight weeks. In certain circumstances it is possible for you to have a removable boot instead of a cast. A member of the foot and ankle team will advise as to whether this option is suitable for you. Footwear is important - it is advisable to wear flat sturdy lace-up shoes, for example, trainers or boots. This will not only support your foot, but will also accommodate orthoses (shoe inserts).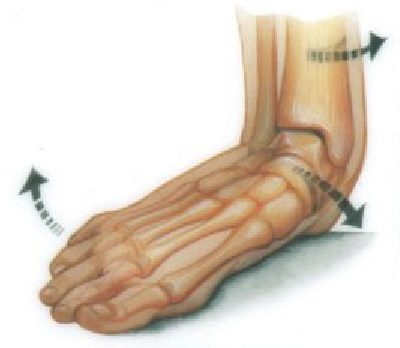
Surgical Treatment
If surgery is necessary, a number of different procedures may be considered. The specifics of the planned surgery depend upon the stage of the disorder and the patient?s specific goals. Procedures may include ligament and muscle lengthening, removal of the inflamed tendon lining, tendon transfers, cutting and realigning bones, placement of implants to realign the foot and joint fusions. In general, early stage disease may be treated with tendon and ligament (soft-tissue) procedures with the addition of osteotomies to realign the foot. Later stage disease with either a rigidly fixed deformity or with arthritis is often treated with fusion procedures. If you are considering surgery, your doctor will speak with about the specifics of the planned procedure.
Adult acquired flatfoot deformity (AAFD) is a painful, chronic condition found most often in women between the ages of 40 and 60. AAFD occurs when the soft tissues of the foot are overstretched and torn, causing the arch to collapse. Flatfoot deformities may also be caused by a foot fracture, or may result from long-term arthritis. Once the posterior tibial tendon-the tendon unit that holds up the arch-loses its function, the foot becomes ?flat? as the bones spread out of position during weight bearing. Without an AAFD repair, the condition may progress until the affected foot becomes entirely rigid and quite painful.

Causes
There are numerous causes of acquired adult flatfoot, including fracture or dislocation, tendon laceration, tarsal coalition, arthritis, neuroarthropathy, neurologic weakness, and iatrogenic causes. The most common cause of acquired adult flatfoot is posterior tibial tendon dysfunction.
Symptoms
Depending on the cause of the flatfoot, a patient may experience one or more of the different symptoms here. Pain along the course of the posterior tibial tendon which lies on the inside of the foot and ankle. This can be associated with swelling on the inside of the ankle. Pain that is worse with activity. High intensity or impact activities, such as running, can be very difficult. Some patients can have difficulty walking or even standing for long periods of time. When the foot collapses, the heel bone may shift position and put pressure on the outside ankle bone (fibula). This can cause pain on the outside of the ankle. Arthritis in the heel also causes this same type of pain. Patients with an old injury or arthritis in the middle of the foot can have painful, bony bumps on the top and inside of the foot. These make shoewear very difficult. Occasionally, the bony spurs are so large that they pinch the nerves which can result in numbness and tingling on the top of the foot and into the toes. Diabetics may only notice swelling or a large bump on the bottom of the foot. Because their sensation is affected, people with diabetes may not have any pain. The large bump can cause skin problems and an ulcer (a sore that does not heal) may develop if proper diabetic shoewear is not used.
Diagnosis
Perform a structural assessment of the foot and ankle. Check the ankle for alignment and position. When it comes to patients with severe PTTD, the deltoid has failed, causing an instability of the ankle and possible valgus of the ankle. This is a rare and difficult problem to address. However, if one misses it, it can lead to dire consequences and potential surgical failure. Check the heel alignment and position of the heel both loaded and during varus/valgus stress. Compare range of motion of the heel to the normal contralateral limb. Check alignment of the midtarsal joint for collapse and lateral deviation. Noting the level of lateral deviation in comparison to the contralateral limb is critical for surgical planning. Check midfoot alignment of the naviculocuneiform joints and metatarsocuneiform joints both for sag and hypermobility.
Non surgical Treatment
The adult acquired flatfoot is best treated early. Accurate assessment by your doctor will determine which treatment is suitable for you. Reduce your level of activity and follow the RICE regime. R - rest as often as you are able. Refrain from activity that will worsen your condition, such as sports and walking. I - ice, apply to the affected area, ensure you protect the area from frostbite by applying a towel over the foot before using the ice pack. C - compression, a Tubigrip or elasticated support bandage may be applied to relieve symptoms and ease pain and discomfort. E - elevate the affected foot to reduce painful swelling. You will be prescribed pain relief in the form of non-steroidal antiinflammatory medications (if you do not suffer with allergies or are asthmatic). Immobilisation of your affected foot - this will involve you having a below the knee cast for four to eight weeks. In certain circumstances it is possible for you to have a removable boot instead of a cast. A member of the foot and ankle team will advise as to whether this option is suitable for you. Footwear is important - it is advisable to wear flat sturdy lace-up shoes, for example, trainers or boots. This will not only support your foot, but will also accommodate orthoses (shoe inserts).
Surgical Treatment
If surgery is necessary, a number of different procedures may be considered. The specifics of the planned surgery depend upon the stage of the disorder and the patient?s specific goals. Procedures may include ligament and muscle lengthening, removal of the inflamed tendon lining, tendon transfers, cutting and realigning bones, placement of implants to realign the foot and joint fusions. In general, early stage disease may be treated with tendon and ligament (soft-tissue) procedures with the addition of osteotomies to realign the foot. Later stage disease with either a rigidly fixed deformity or with arthritis is often treated with fusion procedures. If you are considering surgery, your doctor will speak with about the specifics of the planned procedure.
