Overview
Small or mild length leg discrepancies (LLD), i.e., below 3.0 cm, have been considered as enough to cause orthopaedic changes such as lumbar pain, stress fractures and osteoarthritis on lower limbs (LLLL) joints. In addition to the classification by its magnitude, discrepancies can also be categorized according to etiology, being structural when a difference is noted between bone structures' length or functional as a result of mechanical changes on the lower limb, and are found in 65% - 70% of the healthy population.
Causes
The causes of LLD are many, including a previous injury, bone infection, bone diseases (dysplasias), inflammation (arthritis) and neurologic conditions. Previously broken bones may cause LLD by healing in a shortened position, especially if the bone was broken in many pieces (comminuted) or if skin and muscle tissue around the bone were severely injured and exposed (open fracture). Broken bones in children sometimes grow faster for several years after healing, causing the injured bone to become longer. Also, a break in a child?s bone through a growth center (located near the ends of the bone) may cause slower growth, resulting in a shorter extremity. Bone infections that occur in children while they are growing may cause a significant LLD, especially during infancy. Bone diseases may cause LLD, as well; examples are neurofibromatosis, multiple hereditary exostoses and Ollier disease. Inflammation of joints during growth may cause unequal extremity length. One example is juvenile rheumatoid arthritis. Osteoarthritis, the joint degeneration that occurs in adults, very rarely causes a significant LLD.
Symptoms
The most common symptom of all forms of LLD is chronic backache. In structural LLD the sufferer may also experience arthritis within the knee and hip are, flank pain, plantar fasciitis and metatarsalgia all on the side that is longer. Functional LLD sufferers will see similar conditions on the shorter side.
Diagnosis
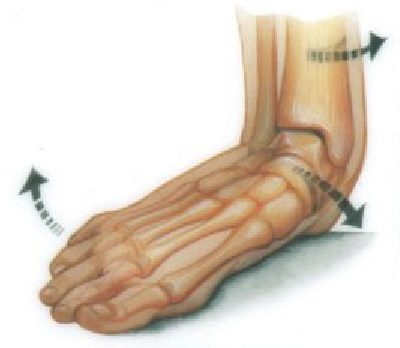
A systematic and well organized approach should be used in the diagnosis of LLD to ensure all relevant factors are considered and no clues are overlooked which could explain the difference. To determine the asymmetry a patient should be evaluated whilst standing and walking. During the process special care should be used to note the extent of pelvic shift from side to side and deviation along the plane of the front or leading leg as well as the traverse deviation of the back leg and abnormal curvature of the spine. Dynamic gait analysis should be conducted during waling where observation of movement on the sagittal, frontal and transverse planes should be noted. Also observe head, neck and shoulder movements for any tilting.
Non Surgical Treatment
The treatment of LLD depends primarily on the diagnosed cause, the age of the patient, and the severity of the discrepancy. Non-operative treatment is usually the first step in management and, in many cases, LLD is mild or is predicted to lessen in the future, based on growth rate estimates in the two legs. In such cases, no treatment may be necessary or can be delayed until a later stage of physical maturity that allows for clearer prognostic approximation. For LLD of 2cm to 2.5cm, treatment may be as simple as insertion of a heel lift or other shoe insert that evens out leg lengths, so to speak. For more severe cases, heel lifts can affect patient comfort when walking, decrease ankle stability, and greatly increase the risk of sprains. For infants with congenital shortening of the limb, a prosthetic ? often a custom-fit splint made of polypropylene ? may be successful in treating more severe LLD without surgery. In many instances, however, a surgical operation is the best treatment for LLD.

Surgical Treatment
The bone is lengthened by surgically applying an external fixation device to the leg. The external fixator, a scaffold-like frame, is connected to the bone with wires, pins, or both. A small crack is made in the bone and the frame creates tension when the patient or family member turns its dial. This is done several times each day. The lengthening process begins approximately five to 10 days after surgery. The bone may lengthen 1 millimeter per day, or approximately 1 inch per month. Lengthening may be slower in a bone that was previously injured. It may also be slower if the leg was operated on before. Bones in patients with potential blood vessel abnormalities, such as cigarette smokers, may also need to be lengthened more slowly. The external fixator is worn until the bone is strong enough to support the patient safely. This usually takes about three months for each inch. Factors such as age, health, smoking and participation in rehabilitation can affect the amount of time needed.
Small or mild length leg discrepancies (LLD), i.e., below 3.0 cm, have been considered as enough to cause orthopaedic changes such as lumbar pain, stress fractures and osteoarthritis on lower limbs (LLLL) joints. In addition to the classification by its magnitude, discrepancies can also be categorized according to etiology, being structural when a difference is noted between bone structures' length or functional as a result of mechanical changes on the lower limb, and are found in 65% - 70% of the healthy population.

Causes
The causes of LLD are many, including a previous injury, bone infection, bone diseases (dysplasias), inflammation (arthritis) and neurologic conditions. Previously broken bones may cause LLD by healing in a shortened position, especially if the bone was broken in many pieces (comminuted) or if skin and muscle tissue around the bone were severely injured and exposed (open fracture). Broken bones in children sometimes grow faster for several years after healing, causing the injured bone to become longer. Also, a break in a child?s bone through a growth center (located near the ends of the bone) may cause slower growth, resulting in a shorter extremity. Bone infections that occur in children while they are growing may cause a significant LLD, especially during infancy. Bone diseases may cause LLD, as well; examples are neurofibromatosis, multiple hereditary exostoses and Ollier disease. Inflammation of joints during growth may cause unequal extremity length. One example is juvenile rheumatoid arthritis. Osteoarthritis, the joint degeneration that occurs in adults, very rarely causes a significant LLD.
Symptoms
The most common symptom of all forms of LLD is chronic backache. In structural LLD the sufferer may also experience arthritis within the knee and hip are, flank pain, plantar fasciitis and metatarsalgia all on the side that is longer. Functional LLD sufferers will see similar conditions on the shorter side.
Diagnosis
A systematic and well organized approach should be used in the diagnosis of LLD to ensure all relevant factors are considered and no clues are overlooked which could explain the difference. To determine the asymmetry a patient should be evaluated whilst standing and walking. During the process special care should be used to note the extent of pelvic shift from side to side and deviation along the plane of the front or leading leg as well as the traverse deviation of the back leg and abnormal curvature of the spine. Dynamic gait analysis should be conducted during waling where observation of movement on the sagittal, frontal and transverse planes should be noted. Also observe head, neck and shoulder movements for any tilting.
Non Surgical Treatment
The treatment of LLD depends primarily on the diagnosed cause, the age of the patient, and the severity of the discrepancy. Non-operative treatment is usually the first step in management and, in many cases, LLD is mild or is predicted to lessen in the future, based on growth rate estimates in the two legs. In such cases, no treatment may be necessary or can be delayed until a later stage of physical maturity that allows for clearer prognostic approximation. For LLD of 2cm to 2.5cm, treatment may be as simple as insertion of a heel lift or other shoe insert that evens out leg lengths, so to speak. For more severe cases, heel lifts can affect patient comfort when walking, decrease ankle stability, and greatly increase the risk of sprains. For infants with congenital shortening of the limb, a prosthetic ? often a custom-fit splint made of polypropylene ? may be successful in treating more severe LLD without surgery. In many instances, however, a surgical operation is the best treatment for LLD.

Surgical Treatment
The bone is lengthened by surgically applying an external fixation device to the leg. The external fixator, a scaffold-like frame, is connected to the bone with wires, pins, or both. A small crack is made in the bone and the frame creates tension when the patient or family member turns its dial. This is done several times each day. The lengthening process begins approximately five to 10 days after surgery. The bone may lengthen 1 millimeter per day, or approximately 1 inch per month. Lengthening may be slower in a bone that was previously injured. It may also be slower if the leg was operated on before. Bones in patients with potential blood vessel abnormalities, such as cigarette smokers, may also need to be lengthened more slowly. The external fixator is worn until the bone is strong enough to support the patient safely. This usually takes about three months for each inch. Factors such as age, health, smoking and participation in rehabilitation can affect the amount of time needed.